Although they are young, children with (bronchial) asthma should understand the lung disease so that they take the therapy seriously and can live well with the respiratory disease.
We explain the most important points about asthma in a child-friendly way.

Has your doctor told you that you have bronchial asthma? Do you now want to understand exactly what that is? Do you wonder how and why you get short of breath and get asthma attacks and what you can do about it? We answer these questions for you.
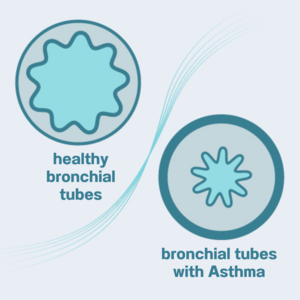
Asthma means that your airways are sick. These airways are called bronchial tubes and are in your lungs. You can imagine the bronchial tubes as small tubes that the air flows through when you breathe in and out.
If your bronchial tubes are healthy, the air can flow through them freely. If you have asthma, these tubes are very sensitive and sometimes get narrower. When the bronchial tubes are narrowed, the air can’t flow freely through them because there is less space. The air has to force its way through them. This is why when you breathe in, less air goes into the bronchial tubes than when they are wide.
Imagine you have a straw in a glass of juice. If the straw is not damaged, you can drink lots of juice through the straw. But if the straw is squashed it takes a lot more effort and takes longer to drink the same amount of juice.
Just as you can suck up less juice through the narrowed straw in the same amount of time, you can breathe in less air through narrowed bronchial tubes than through wide ones.
Are you now wondering why your bronchial tubes get narrower? There are three reasons for this. To help you understand better, we will first explain how your bronchial tubes are constructed.
The tubes in your airways, your bronchial tubes, have walls. These are called bronchial walls. The walls are made up of a layer of muscle (= bronchial muscles), the mucous membrane and a thin layer of mucus. Everyone’s bronchial tubes are made up like this – including yours.
But bronchial asthma narrows the bronchial tubes because
This all happens because your bronchial tubes are very sensitive and overreact to things that are harmless to healthy people.
When you have an asthma attack, your sensitive bronchial tubes are overreacting to one of these harmless triggers. Within just a few minutes, the mucous membrane swells and the bronchial muscles seize up. This narrows your “breathing tubes” and so the air cannot flow through them as easily. This causes shortness of breath, triggers a cough or, if it is a very bad asthma attack, makes you feel as if you are not able to breathe at all.
Everyone with asthma will have different things that trigger the shortness of breath. How severely something irritates the bronchial tubes and how bad the asthma attack is varies from one person to another and from one situation to another.

It is important for you to know what triggers your asthma. Because then you can avoid these triggers and prevent an asthma attack.
You can find out what triggers your asthma. A trigger is something that makes your asthma worse or causes an attack. To do this, you can keep an asthma diary where you can write down extra information when you have had an attack:
As well as shortness of breath, where you feel as if you cannot breathe, there are also other signs of asthma. A dry cough is typical and so are noises when you breathe, like whistling—also called wheezing—and in rare cases, a rattling sound.
Signs of asthma at a glance:

Your doctor will tell you what you can and have to do against your asthma.
Usually asthma therapy involves the following:
If your asthma is well-managed and you do your inhalation therapy regularly, your respiratory disease will not really bother you too much in your day-to-day life.
Note: The information in this blog post is not a treatment recommendation. The needs of patients vary greatly from person to person. The treatment approaches presented should be viewed only as examples. PARI recommends that patients always consult with their physician or physiotherapist first.
An article written by the PARI BLOG editorial team.
© 2025 PARI GmbH Spezialisten für effektive Inhalation