
A cough with sputum, also known as a productive cough, is the body’s defence mechanism to keep the airways clear. What are the causes? What does the colour of the mucus mean? What can you do against secretions when you cough? Here are some tips and information.
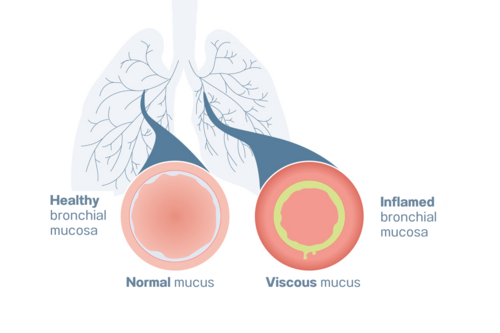
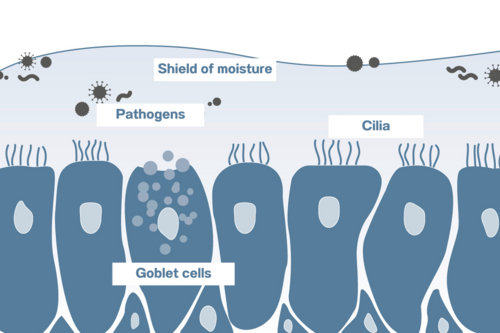
If your airways are infected, for example if you have acute bronchitis or an RSV (Respiratory Syncytial Virus) infection, the bronchial tubes produce more mucus – and this is why there is sputum when you cough. A cough is the body’s defence mechanism for transporting pathogens, pollen or other foreign particles out of the bronchial tubes with the aid of mucus.
The cough reflex ensures that we cough and that the mucus can be released from the bronchial walls. The secretions and all of the pathogens trapped inside are propelled out of the airways towards the mouth and are then ideally spat out.
Lung specialist Prof. Fischer says: “If you have a cough with sputum, it is best to spit out the mucus, as its colour and consistency can tell us doctors a lot about possible diseases such as asthma or a bacterial infection. But it is also safe to swallow because the mucus is broken down in the stomach and is digested. It is not harmful to your health if you swallow it, but spitting it out can be of diagnostic value.“

Whether a cough with sputum is dangerous depends on factors such as the underlying triggers, how long the cough lasts, the amount and colour of the secretion and the other symptoms. Only a doctor can assess how dangerous the phlegmy cough is.
A cough is classified as productive – which means a cough with more sputum than expected – if you cough up more than about 2 tablespoons of mucus within 24 hours. If you feel like you have a build-up of mucus, it is therefore advisable to spit out the secretions so that you can better assess how much there is and tell your doctor the next time you see them.
If you have the following symptoms, you should immediately see a doctor:
There are many different causes of a productive cough (= cough with sputum). The most common of these are:
The colour of the sputum may give an indication of the underlying disease:
If your mucus is an unusual colour, you should contact your doctor. They can send your sputum (= the mucus you spit out) to a laboratory to test it for bacteria, fungi or other germs – and may arrange further testing.
Prof. Fischer explains when pulmonary practices send secretions to the lab: “It is difficult to define when the sputum should be sent for testing. If it is yellowish or greenish, which is a sign of bacterial colonisation consistent with acute bronchitis, you don’t usually take a bacterial profile. We know that we can generally use antibiotic treatment here because this reaches most gram-positive bacteria. It is a similar situation for a quote unquote normal lung infection. But if the patient does not respond to the treatment and there is some uncertainty, it makes sense to run additional microbiological tests. But this is only if the sputum comes from deep in the airways and is not just saliva. The sputum sample also needs to reach the laboratory quickly and be tested promptly once it arrives so that the results are actually conclusive.”
There are things you can do yourself to tackle a cough with sputum. Many of these recommendations are also advocated by doctors as part of medically prescribed therapies.
Inhalation therapy of saline solutions with a nebuliser can help liquify the mucus and calm the airways. The fine aerosols penetrate into the bronchial tubes (unlike steam inhalation) and coat the mucus and mucous membranes like a film. The saline solution liquifies the mucus, which makes it easier to cough up. Inhalation devices, such as those from PARI, offer specialised products for various diseases – both for adults and for children.
Inhalation therapy with hypertonic saline solutions is ideal for a cough with sputum. Hypertonic saline solutions are especially effective at breaking up thick mucus in the bronchial tubes. This is because the principle of osmosis comes into play with the 3% and 6% solutions. Here, water is withdrawn from the cells of the mucous membranes. This water then passes into the mucus coating the mucous membranes. The mucus is liquified, which is why it is then easier to cough up. Here, it is important to note that the higher the salt content, the more effectively the mucus will be broken up and the stronger the urge to cough will be.

Respiratory therapy devices such as the PARI O-PEP use vibrations and air resistance to help release the mucus from the bronchial walls. When you breathe out through the device, the air and airways start to vibrate slightly. In the same way as shaking a bottle of ketchup helps mobilise the ketchup, the vibrations set the secretions in the lungs in motion. The increased resistance as you exhale also expands the bronchial tubes, which promotes ventilation of the lungs.
There are simple breathing and mobilisation exercises that help ventilate the lungs and support the transport of secretions out of the lungs as a result of coughing with sputum. These include breathing techniques such as pursed lip breathing and these 8 exercises to clear mucus from the lungs.
You should drink plenty if you have a cough with mucus. Ideal drinks are still water, herbal teas or fruit juice diluted with sparkling water. This method moistens the mucous membranes from the inside out, making secretions less sticky and thick.
You may also be interested in these blog posts about lung health and coughs:
Note: The information in this blog post is not a treatment recommendation. The needs of patients vary greatly from person to person. The treatment approaches presented should be viewed only as examples. PARI recommends that patients always consult with their physician or physiotherapist first.
An article written by the PARI BLOG editorial team.
© 2025 PARI GmbH Spezialisten für effektive Inhalation